SARS-CoV-2 Immunogenity at the Crossroads
The current coronal virus 2 pandemic presents a world-wide health risk. Researchers at the Paul-Ehrlich-Institut, Federal Institute for Vaccines and Biomedicines (PEI) have summarised the latest findings on the function, structure, and immunogenicity of the spike protein (surface protein of the virus) as well as occurring mutations and the significance for the development of vaccines and therapeutics in a current publication (Allergy, online edition of 13 May 2020).
The new coronavirus SARS-CoV-2 can lead to serious disease courses due to misguided reactions of the immune system including a lung inflammation which can lead to lung failure and death. The virus is being intensively investigated, attempts are made to find specific characteristics, which could on the one hand explain the transmissibility and the differences in the clinical course of the COVID-19 disease, and on the other hand, provide approaches for the development of vaccines and therapies. In this context, efforts are also made to identify the specific differences between COVID-19 and the closely related SARS coronavirus SARS-CoV-1, which caused the pandemic outbreak of 2002/2003.
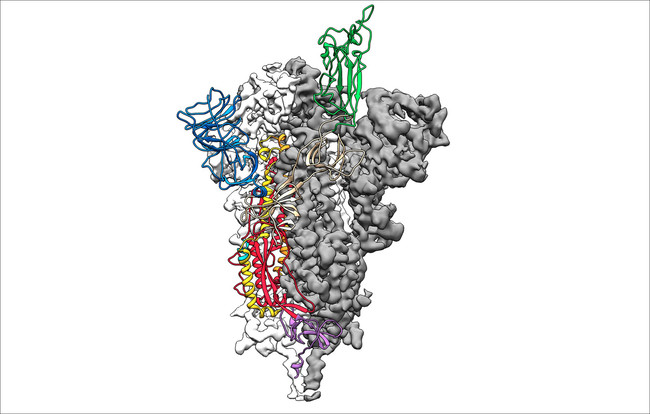
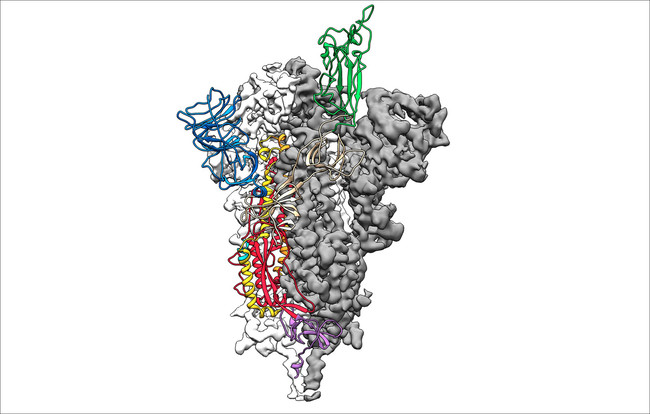
As in other coronaviruses, the entry of the virus into the cell requires the co-ordinated action of receptor binding and proteolytic processing of the trimer surface spike glycoproteins (s), which was identified as the central antigen for the development of vaccines.
The differences identified between SARS-CoV-2 and SARS-CoV-1 include a different proteolytic cleavage site at the transition of the spike protein sub-units S1 to S2 (monobasic cleavage site for SARS-CoV-1 compared with polybasic furin cleavage site for SARS-CoV-2). This could cause existing furin proteases to contribute to entering the SARS-CoV-2 into quite different tissues thus enabling the virus to spread more effectively than SARS-CoV-1, which is also of significance for the clinical course of infections.
For vaccine development, it is above all important to understand the structure of the S-protein of the new SARS-CoV-2 virus. Of interest, in this context, are certain epitopes, i.e. segments of molecule against which antibodies or T-cells are formed during an immune response. According to predictions, there are specific epitopes, which are highly preserved between SARS-CoV-1 und SARS-CoV-2. This could mean that vaccines targeted to such epitopes could have a cross-protective effect, i.e. confer protection against different coronaviruses and newly occurring virus mutations.
Which therapeutic approaches will be pursued and which ones are considered as promising? The majority of all vaccine strategies which are already being investigated in clinical studies are aimed at the S-protein as the ideal candidate protein (antigen) for conferring vaccine protection. As a therapeutic option for the treatment of COVID-19 disease, antibodies that prevent the transmission of viruses in the human body from cell to cell, so-called neutralizing antibodies, are currently being tested. These are contained in convalescent plasmas, but can also be neutralizing monoclonal antibodies or antibody cocktails. Immunomodulatory monoclonal antibodies are also being tested to alleviate the observed cytokine storm, reduce excessive inflammatory reactions and thus counteract lung damage.
Original Publication
Karamloo F, König R (2020): SARS-CoV-2 immunogenicity at the crossroads.
Allergy 75: 1822-1824.
Online-Abstract
top